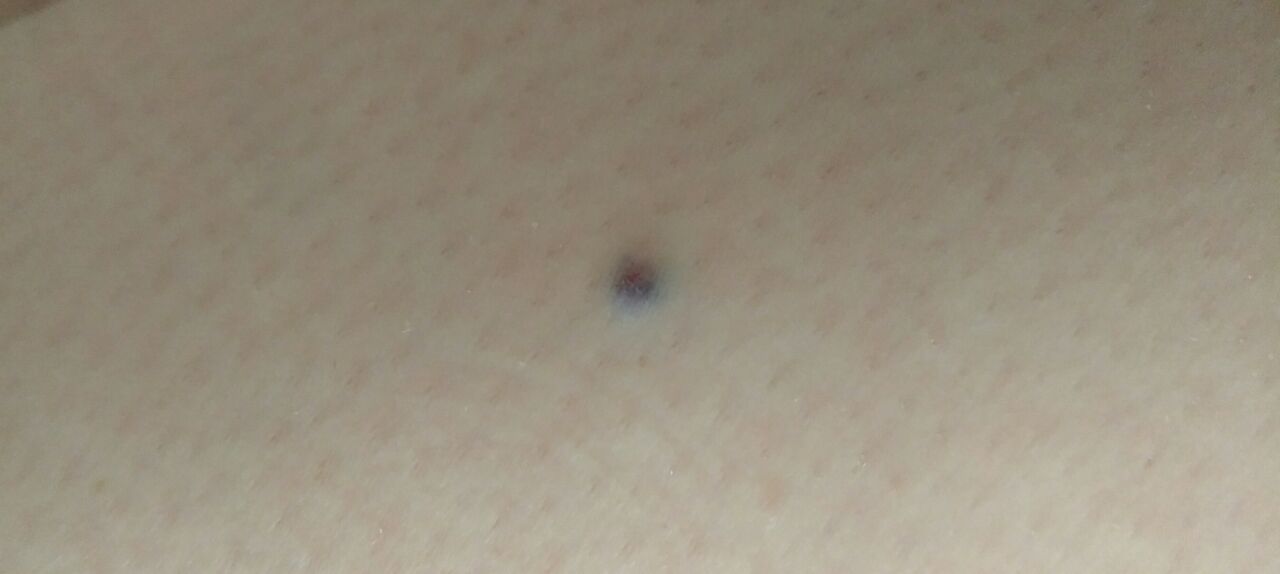
Blue nevus (blue nevus of Jadassohn–Tièche, blue neuronevus, dermal melanocytoma) is a benign skin neoplasm with a characteristic color from blue to dark blue. The appearance of blue nevus is usually observed during puberty, but can occur at any other age (including being congenital). Multiplicity is rare. By gender, blue nevi are more often observed in women compared with men.
Predisposing factors
There is no clear reason for the appearance of blue nevi. It is only appropriate to talk about predisposing factors that, to varying degrees, can increase the risk of neoplasms:
- Genetic factor: the appearance of blue nevi can be due to the human genome;
- Ultraviolet radiation: artificial or solar ultraviolet leads to faster reproduction of nevoid cells (nevus cells) and excessive production of melanin (pigment, the accumulation of which is noted in nevus);
- Hormonal changes: hormonal fluctuations in the body (especially sex hormones, thyroid hormones and adrenal hormones) can affect the appearance of new nevi and the growth of existing ones;
- Ionizing radiation, viral diseases, and injuries can also provoke the appearance or growth of blue nevi.
Diagnostics
The diagnosis of blue nevi is based on a clinical examination, which includes a routine examination of the formation and dermatoscopy. If you suspect malignant growth, a biopsy can be performed.
Symptoms
On visual inspection of the blue nevus, a spot or slightly elevated nodule is determined. Most often, the formation is symmetrical (oval or round, sometimes spindle-shaped). The surface of the nevus can be a texture of ordinary skin, a smooth skin pattern (up to a glossy surface), or tuberosity (large nevi, over 10 mm in diameter).
The borders of the blue nevus are fuzzy (blurry), but usually smooth. Rarely, an uneven edge can be observed in formations with a large diameter (an unfavorable sign). The color of the blue nevus varies from blue to dark blue (including gray-blue, blue-brown shades), which is associated with a deep occurrence of pigment in the skin. In the distribution of pigment by formation, a gradual decrease in the color intensity is observed in the direction from the center to the periphery; in large nevi, there may be heterogeneity of color over the entire area, spotting (polychrome).
Hair is most often absent, sometimes can be observed on the periphery.
The dimensions of the blue nevus usually do not exceed 10 mm. Growth is slow. Formations over 1 cm are very rare (blue cell nevus).
On palpation of a simple nevus, there are no features: the consistency of ordinary skin or somewhat denser (large, protruding forms over the skin). Subjective sensations are absent.
Neoplasms are located mainly on the trunk, limbs, or neck, rarely on the head. Typical localization of large cell nevus is the sacro-gluteal region.
Dermatoscopic Description
With dermatoscopy of the blue nevus, the following is visualized:
- Symmetry;
- Lack of clear boundaries;
- Gradual decrease in color intensity from the center to the periphery;
- Homogeneous structureless pigmentation of a gray-blue color (a consequence of the occurrence of melanocytes in the papillary (gray) and reticular (blue) layers of the dermis);
- Polychrome, color heterogeneity, vessels, and globules are rare signs of blue nevi.
Differential diagnosis
Differential diagnosis is carried out with such neoplasms as:
- Post-inflammatory hyperpigmentation;
- Congenital dermal melanocytosis;
- Pigmented nevus (simple or papillomatous);
- Hemangioma;
- Spitz Nevus;
- Dysplastic nevus;
- Melanoma.
Risks
In most cases, the blue nevus is safe. However, compared with simple pigmented nevus, the risk of melanoma on the background of blue nevus is slightly higher: less than 1% and 3%, respectively. Signs of a possible malignancy: a change in appearance, the appearance of subjective sensations.
Tactics
In the absence of any damaging effect on the blue nevus, changes in appearance and subjective sensations, self-control (or inspection with the help of other persons in inaccessible areas) is enough at least once a year. If mechanical damage to the nevus has occurred, its active irradiation with ultraviolet or ionizing radiation, as well as if any changes in the nevus itself are noticed or previously absent sensations appear, you need to consult a dermatologist or oncologist.
The specialist determines the possibility of further dynamic monitoring (terms are determined individually) or indications are made for the removal of the damaged nevus. It is necessary to remove those nevi that are subject to constant, chronic trauma to clothing, jewelry, or due to the characteristics of professional employment.
In the case of dynamic observation, photo fixation of skin neoplasms is of great value, which will subsequently determine even minor changes in the appearance of the nevus.
Patients with blue nevus on the skin are shown an examination by a dermatologist or oncologist in the spring and autumn (before and after the beach season). Mapping of skin neoplasms is also recommended, which greatly simplifies further observation, the search for new formations, or changes to existing ones.
Treatment
Only surgical (classic, using an electric or radio scalpel) with a mandatory histological examination.
Treatment of blue nevus using destructive methods (laser removal or cryodestruction) is not recommended.
Prevention
Prevention of the appearance of nevi and their malignancy consists in a gentle and careful attitude to the skin:
- Limitation of ultraviolet radiation (tanning bed, solar tanning);
- The use of protective creams during periods of active sun;
- Exclusion of chronic skin trauma;
- Limitation or exclusion of ionizing radiation, occupational hazards;
- Compliance with safety measures when working with skin-damaging factors;
- Personal hygiene and basic awareness of skin tumors.
A regular examination of the blue nevi, timely consultation of a specialist in the event of external changes, and removal of potentially dangerous neoplasms are also required.