Seborrheic keratosis (seborrheic wart, senile wart, senile keratosis, senile keratoma) is a benign tumor rising above the skin with keratinization. These formations appear, as a rule, over the age of 50 years. Seborrheic keratosis is characterized by plurality, the proportion of which increases with age. Equally common in both men and women.
Predisposing factors
There is no clear reason for the appearance of seborrheic keratosis. It is only appropriate to talk about predisposing factors that, to varying degrees, can increase the risk of neoplasms:
- Involute (age-related) skin changes, with histological and functional changes: aging of epidermal keratinocytes with late apoptosis;
- Excessive insolation;
- Genetic factor: the appearance of seborrheic keratosis may be due to the human genome;
- Ionizing radiation and viral diseases can also provoke the appearance or growth of keratomas.
Diagnostics
The diagnosis of seborrheic keratosis is based on a clinical examination, which includes a routine examination of the formation and dermatoscopy. If you suspect malignant growth, a biopsy can be performed.
Symptoms
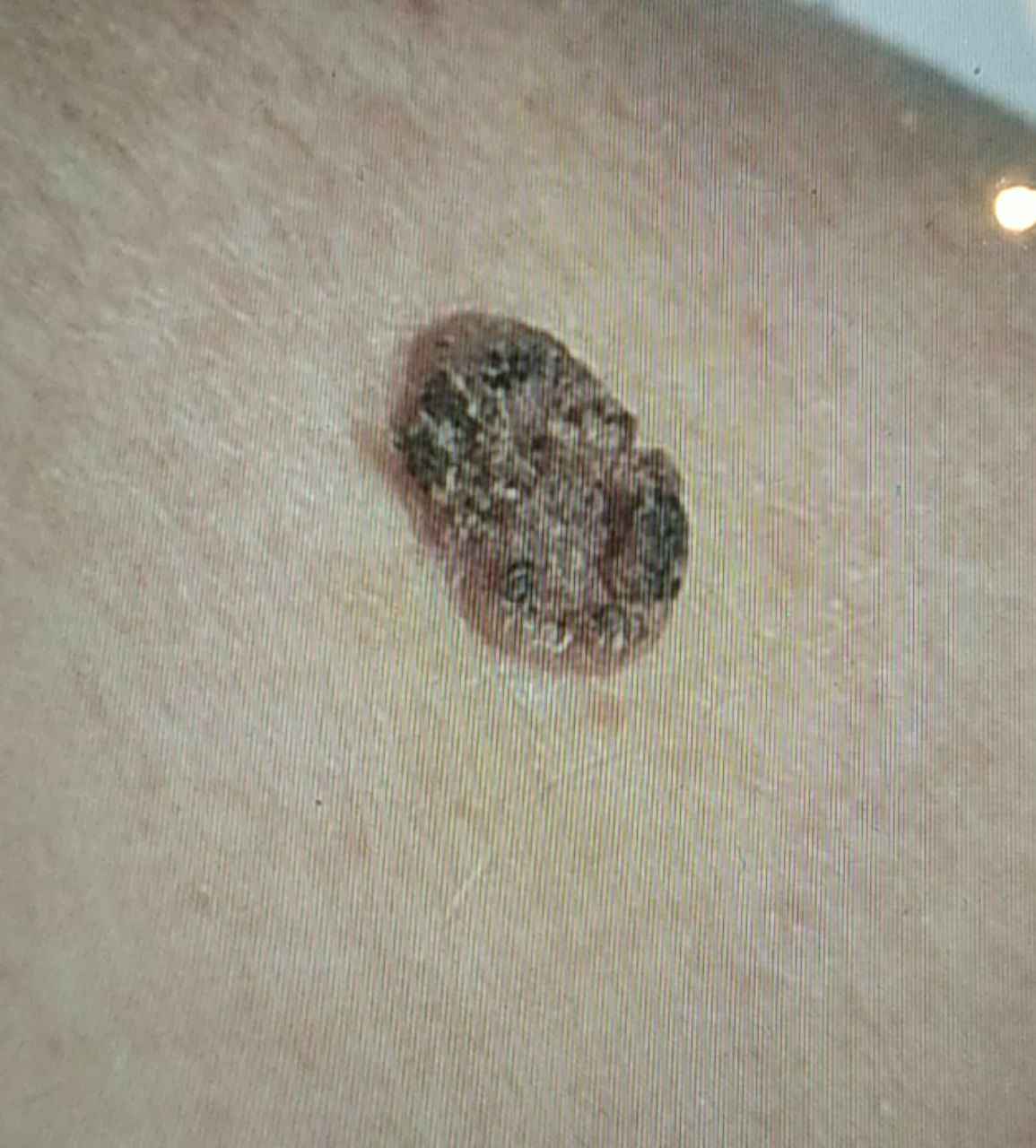
A visual examination of seborrheic keratoma reveals a flattened, hemispherical, or short wide leg formation that rises above the skin, most often symmetrical (oval or round). The surface of keratoma differs significantly from the texture of ordinary skin: rough, dry, with peeling, warty (in the form of large, uneven dry papillae). Rough surfaces are more characteristic for formations over 10 mm. Sometimes keratinization is so strong that keratoma fragments can fall off on their own or with little physical impact.
The boundaries of senile keratoma are clear and even. The color is nude, gray, gray-brown. Sometimes pink or pink-red shades are present. Redness of unchanged skin around the formation itself may be noted.
The presence of keratoma does not affect hair growth.
Sizes range from 5 mm to 20 mm. Formations over 15 mm are rare. The height of such a nevus above the skin does not exceed 5-7 mm.
On palpation, a dense, dry formation with peeling is determined. Subjective sensations are usually absent or mild itching.
Keratomas are located mainly on the trunk, upper limbs. They can be located on the face, scalp, neck, lower extremities.
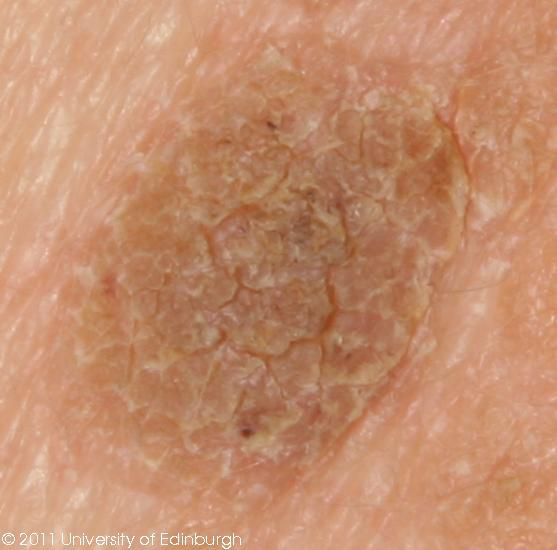
Dermatoscopic Description
With dermatoscopy of seborrheic keratoma, the following signs are visualized:
- Homogeneous background pigmentation from pale gray to brown;
- Comedone-like structures: clear gray-brown keratotic inclusions of the correct form;
- Milium-like cysts: spherical structures of a dull white color or with a yellowish tinge;
- Blood vessels in the form of a hairpin;
- Structures resembling the convolutions of the brain;
- Evenly colored pseudo-network with uneven, sharply breaking off edges (typical for the face);
- Uniform dot pigmentation of gray-black color.
Differential diagnosis
Differential diagnosis is carried out with such pigmented neoplasms, as:
- Actinic keratosis;
- Papillomatous nevus;
- Dermatofibroma;
- Bowen’s disease;
- Keratoacanthoma;
- Basal cell carcinoma;
- Squamous cell carcinoma;
- Melanoma.
Risks
Seborrheic keratosis is an optional precancerous condition. Malignancy occurs rarely and is more often observed under the influence of additional factors (chronic injury, thermal and chemical burns). The risk of malignant transformation is 1-10%. In the case of malignancy, seborrheic keratosis is more often transformed into squamous cell (squamous) cancer. Sometimes this happens through a clinically determined phase of Bowen’s disease.
It should be carried in mind that patients with a large number of keratomas have an increased risk of a malignant tumor on unchanged skin or near keratoma. This can complicate the timely detection and differential diagnosis of tumors.
Tactics
In the absence of any damaging effect on seborrheic keratoma, changes in appearance and subjective sensations, self-control (or examination with the help of other persons in inaccessible areas) is enough at least once a year. If mechanical damage has occurred, active exposure to ultraviolet or ionizing radiation, as well as if any changes in the keratoma itself have been noticed or previously absent sensations have appeared, a dermatologist or oncologist needs to be consulted.
The specialist determines the possibility of further dynamic observation (terms are determined individually) or indications are set for the removal of damaged skin formation. It is necessary to remove those keratomas that are subject to constant, chronic trauma to clothing, jewelry, or due to the characteristics of professional employment.
In the case of dynamic observation, photo fixation of skin neoplasms is of great value, which will subsequently determine even minor changes in appearance.
Patients with seborrheic keratosis are shown an examination by a dermatologist or oncologist in the spring and autumn (before and after the beach season). Such patients are recommended to compile a map of skin neoplasms, which greatly simplifies further observation, the search for new formations, or a change in existing ones.
Treatment
Treatment can be surgical or using local destruction methods (laser, cryodestruction). After surgical treatment (classical, with the help of an electric or radio scalpel), histological examination is mandatory.
The use of laser removal or cryodestruction is carried out after a mandatory examination by an oncologist and the exclusion of malignancy. The use of such methods is also not recommended if it is impossible to conduct a clear differential diagnosis with neoplasms of a pigmented nature (pigmented, dysplastic and other nevi).
Prevention
Prevention of the appearance of seborrheic keratosis and its malignancy is gentle and careful attitude to the skin:
- Limitation of ultraviolet radiation (tanning bed, solar tanning);
- The use of protective creams during periods of active sun;
- Exclusion of chronic skin trauma;
- Limitation or exclusion of ionizing radiation, occupational hazards;
- Compliance with safety measures when working with skin-damaging factors;
- Personal hygiene and basic awareness of skin tumors.
It also requires regular examination by keratitis, timely consultation of a specialist in the event of external changes, and the removal of potentially dangerous neoplasms.