Pustular psoriasis is a form of psoriasis (referred to as an independent disease by some medical schools), a chronic inflammatory skin disease that is the presence of white pustules on the skin. Has a more severe course compared to simple psoriasis.
The key point in the diagnosis is the clinical picture and the patient’s complaints in conjunction with typical pathognomonic (specific for pustular psoriasis) signs.
The main therapeutic principles include keratolysis (with the help of urea or salicylic acid preparations), as well as a decrease in the inflammatory response and hyperproliferation of keratinocytes (includes local and systemic treatment with various groups of drugs).
There are several types of pustular psoriasis:
- Generalized pustular psoriasis (von Zumbusch pustular psoriasis);
- Palmoplantar psoriasis (chronic persistent palmoplantar pustulosis, Barbera pustular psoriasis, limb pustular psoriasis);
- Annular pustular psoriasis, or annular pustulosis;
- Acrodermatitis chronica atrophicans (palmar and plantar psoriasis);
- Impetigo herpetiformis.
Etiology (causes)
Unlike psoriasis vulgaris, the cause of pustular psoriasis is unknown. The relationship with trigger factors has not been established or proven insufficient. Somewhat more often, this type of psoriasis occurs in people who smoke. Genetic causes are also rare.
Sometimes pustular psoriasis forms against the background of common, vulgar psoriasis. Factors provoking the transformation of psoriasis vulgaris into pustular psoriasis include:
- Taking a number of drugs: systemic corticosteroids, cytotoxic drugs, salicylates, antidepressants, hydroxychloroquine, calcipotriol, chemotherapy drugs, anabolics, uncontrolled NSAIDs, penicillin antibiotics, progesterone, beta-blockers, oral contraceptives.
- Powerful skin irritants: chemical, biological, physical;
- Severe stress;
- Conditions leading to suppression of immunity (infectious and other severe concomitant diseases);
- Long-term exposure to sunlight, ultraviolet light.
Clinical picture
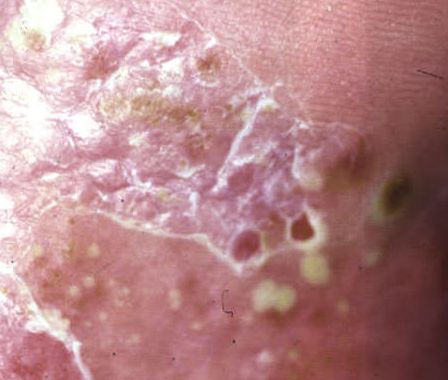
Pustular psoriasis is manifested by the presence of raised vesicles or blisters (pustules) on the surface of the skin, which are filled with a clear liquid (exudate). The skin around is not changed, however, under and above the surface of the pustules and around them, the skin is red, of a higher temperature, swollen, inflamed and thickened, easily exfoliates.
In the case of the addition of a secondary infection (infection of the pustules), the contents become more turbid (up to the appearance of purulent discharge), the signs of inflammation are more pronounced.
Pustular psoriasis is located most often on the distal ends of the limbs (arms and legs), that is, on the legs and forearms. This form is called palmoplantar pustulosis (localized pustular psoriasis).
In more severe cases, pustular psoriasis can be generalized, with widespread pustules over the entire surface of the body and a tendency to merge into larger pustules.
Psoriasis is a chronic disease with a recurrent course: periods of exacerbation are replaced by asymptomatic intervals of varying duration.
Diagnostics
Typically, the diagnosis of pustular psoriasis is clinical. The physical examination is based on examination and identification of the characteristic psoriatic pustules.
Characteristic psoriatic plaques can also be detected, and there is the psoriatic triad of Auspitz:
- The “stearin spot” phenomena (free discharge of scales from the surface of papules);
- The phenomenon of the “terminal film” (reddish shiny surface in the place of removed scales);
- The phenomenon of capillary bleeding (after scraping the red surface, pinpoint bleeding occurs).
In doubtful cases, a biopsy of the affected skin area can be performed for histological confirmation of the diagnosis, as well as culturing of contents from vesicles or blisters.
Differential diagnosis
Pustular psoriasis must be differentiated from diseases such as dermatophytosis of the hands and feet, eczema of the hands and feet, dyshidrotic eczema, keratoderma, toxicoderma, squamous-hyperkeratotic forms of mycosis of the feet and palms.
Generalized pustular psoriasis is differentiated from bacteremia and sepsis by blood.
Psoriasis treatment
The main goal of treatment for pustular psoriasis is to reduce the severity of symptoms and improve the patient’s quality of life.
The basic principles of therapy include:
- Primary keratolysis as a basic local therapy (preparations containing urea and salicylic acid, moisturizing creams);
- Decreased keratinocyte proliferation activity;
- Reducing the severity of the inflammatory process on the skin.
As a local treatment, in addition to basic drugs (urea + salicylic acid), calcineurin inhibitors, topical glucocorticoids, calciferol, and retinoids are prescribed.
The indications for the appointment of systemic therapy are:
- Severe pustular psoriasis;
- Psoriatic arthritis;
- Inadequate response to topical treatment or phototherapy.
In this case, retinoids, fumaric acid esters, immunosuppressants, biotherapy (adalimumab, secukinumab, apremilast, etc.) are prescribed. Also, detoxification therapy is prescribed, correction of vital blood parameters and the function of other organs.
In physiotherapy, phototherapy seems to be the main focus.
Complications
Complications are more pronounced and dangerous compared to psoriasis vulgaris. Against the background of pustular psoriasis, the following complications can develop:
- Pyoderma – purulent skin diseases;
- Alopecia – hair loss and damage;
- Onycholysis – destruction of the nail plate;
- Decrease in the level of albumin and the level of calcium in the blood and their consequences depending on the severity of the deficiency;
- Kidney damage up to renal tubular necrosis with the development of renal failure;
- Liver failure.
Severe complications of generalized pustular psoriasis can cause severe intoxication with subsequent multiple organ failure and death. Complications occur in 17%, deaths occur in 2% of cases.
Prevention
To reduce the risk of developing pustular psoriasis and, to a greater extent, to prevent exacerbations, it is recommended to avoid trigger factors, smoking, excessive alcohol consumption, exclude mechanical skin irritants, monitor body weight, lead a healthy lifestyle (regular physical activity), timely treat concomitant diseases and exclude uncontrolled intake of medicines (without a doctor’s prescription).