Plantar wart (plantar viral wart) is a benign neoplasm towering above the skin located on the plantar surface of the foot. Viral warts are most often found in children and adolescents: skin neoplasms can be found in almost 10% of this age category. This type of neoplasm is characterized by multiplicity, spontaneous involution (observed in 40% of cases, especially in adolescents), resistance to conservative treatment (increases with age).
Predisposing factors
The cause of the appearance of warts is the human papillomavirus (HPV), a predominantly low oncogenic risk. However, given the fact that almost 90% of the entire population shows the carrier of this virus, but not everyone has warts, it is obvious that there are other factors predisposing to the occurrence of these neoplasms on the skin.
Predisposing factors, which to varying degrees can increase the risk of neoplasms, include:
- Immunodeficiency states;
- Overweight;
- Metabolic disorders in the body (e.g., diabetes mellitus);
- Severe infectious diseases;
- Poor personal hygiene;
- Pregnancy;
- Stress, overwork, malnutrition – all that leads to a decrease in the protective properties of the body;
- Chronic skin lesions (like the entrance gate for HPV).
Diagnostics
The diagnosis of warts is based on a clinical examination, which includes a routine examination of the formation and dermatoscopy. To search for HPV, there are a number of tests that are conducted by many laboratories. If malignant growth is suspected, a biopsy can be performed.
Symptoms
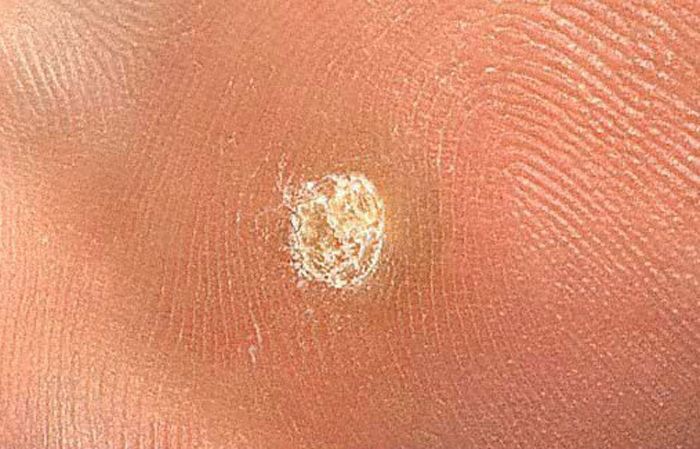
A visual examination of the plantar wart determines a flattened, slightly rising above the skin formation. The surface of the wart is uneven, finely tuberous, in the form of small papillae, rough, with keratinization.
The borders of the wart are clear and even. Usually, the border is represented by a clear “cliff” of the uppermost layers of the skin epidermis (epithelial corolla from the side of healthy skin). The color of the wart is corporal or somewhat paler, in the presence of significant keratinization – there are shades of gray.
There is no hair growth in the wart area. However, this is more due to the fact that the area of the plantar wart does not grow hair on its own.
The size of the warts is small. The diameter is usually 2-5 mm. Large warts are rare (usually these are groups of individual neoplasms merged into one conglomerate).
On palpation, the wart is denser than normal skin. Subjective sensations are also absent, but tingling is often felt with pressure.
Plantar warts are located on the plantar surface of the feet or on the transition zone to the back surface of the foot.
Dermatoscopic Description
The following structures are visualized with dermatoscopy of a plantar wart:
- The symptom of “frogspawn” is a group of densely packed tubercles, each tubercle is represented by the peripheral part of white color (keratinocytes) and the central part in the form of a red dot (feeding vessel). In connection with the expressed pressure of body weight on the wart, the tubercles can be arranged in irregular groups, between which there is a structureless zone of a yellowish tint (hyperkeratosis);
- Black-brown dots can be visualized instead of red dots, – a characteristic sign of thrombosed wart capillaries;
- On the periphery of the wart – a sharp transition to healthy skin, a pale corolla from the horn masses may be located in this area;
- Linear stripes can be present over the entire area of the flat wart – formed as a result of high pressure of the bodyweight on the wart.
Differential diagnosis
Differential diagnosis is carried out with such neoplasms as:
- Pigmentary nevus;
- Nevus of the sebaceous glands;
- Dermatofibroma;
- Corn;
- Flat wart;
- Vulgar wart;
- Molluscum contagiosum;
- Nodal form of basal cell carcinoma;
- Pigmentless melanoma.
Risks
An oncological plantar wart is safe and does not carry an increased risk of malignancy. In the absence of an external effect on such a neoplasm (trauma, ultraviolet radiation, ionizing radiation), the risk of malignancy is comparable to the risk of a malignant tumor on unchanged skin. Signs of a possible tumor degeneration: rapid growth, increase in density, change in appearance, the appearance of subjective sensations.
Plantar warts, given their location, are more dangerous due to their tendency to injure. As a result, there is bleeding, soreness, the resulting wound can become the entrance gate for pathogenic microflora.
Intact warts cause psychological and cosmetic discomfort.
Given the viral nature of these neoplasms, with their multiple appearances it is appropriate to talk about a decrease in the protective properties of the immune system, carriage of HPV. Since HPV can have a high oncogenic risk, it is necessary to be more attentive to one’s health and undergo routine oncological examinations by specialists in a timely manner.
Tactics
In the absence of any damaging effect on the wart, changes in appearance and subjective sensations, self-control (or examination with the help of other persons in inaccessible areas) is enough at least once a year.
If mechanical damage to the wart, active irradiation with ultraviolet or ionizing radiation, as well as if any changes in appearance or previously absent sensations have occurred, you need to consult a dermatologist or oncologist.
The specialist determines the possibility of further dynamic monitoring (the timing is determined individually) or indications are made for the removal of the damaged wart. It is necessary to remove those neoplasms that are subject to constant, chronic trauma to clothing, jewelry, or due to the characteristics of professional employment. Removing warts can be done simply at the request of the patient when they present a cosmetic defect or psychological discomfort.
In the case of dynamic observation, photo fixation of skin neoplasms is of great value, which will subsequently determine even minor changes in appearance.
Patients with multiple neoplasms are shown a dermatologist examination in the spring and autumn (before and after the beach season). Such patients are also recommended to compile a map of skin neoplasms, which greatly simplifies further observation, the search for new formations, or a change in existing ones.
Treatment
Less traumatic methods can be used to treat plantar viral warts:
- Laser removal;
- Cryodestruction with liquid nitrogen;
- Removal with a radio wave scalpel;
- Electrocoagulation
If it is impossible to conduct a less traumatic treatment, as well as in the presence of doubts as to the nature of the neoplasm, the usual surgical treatment is used by excision followed by histological examination of the obtained material.
Self-removal or “removal” of warts cannot be carried out due to the high risk of complications (bleeding, inflammatory processes), as well as the inability to unambiguously independently determine the nature of the removed tumor.
After removal of the warts, in connection with their viral etiology, there is always a risk of the reappearance of similar neoplasms both in the removal area and in adjacent areas. Prevention helps reduce the likelihood of relapse.
Prevention
Prevention of the appearance of warts consists in a gentle and careful attitude to the skin, timely treatment of infectious diseases (including the human papillomavirus, with confirmation of its presence in the body), strengthening immunity, proper and high-quality personal hygiene, and maintaining a healthy lifestyle.
To exclude negative consequences, including malignancy, after the appearance of a wart, it is necessary:
- Limitation of ultraviolet radiation of the corresponding area (tanning bed, solar tanning);
- The use of protective creams during periods of active sun;
- Exclusion of chronic skin trauma;
- Limitation or exclusion of ionizing radiation, occupational hazards;
- Compliance with safety measures when working with skin-damaging factors;
- Personal hygiene and basic awareness of skin tumors.
It also requires regular inspection of warts, timely consultation of a specialist in the event of external changes, and the removal of potentially dangerous neoplasms.