Eczema is the common name for various inflammatory skin diseases characterized by severe itching, peeling and reddening of the skin, and dry or soaking rashes. Eczema is not transmitted by contact with a sick person. It can be acute or chronic, and in most cases is characterized by an improvement in the summer and a worsening in the winter.
Acute eczema is characterized by itching, redness, swelling of the skin and the formation of transparent blisters. Chronic eczema is characterized by redness, a fine rash with peeling and cracking. Due to mechanical irritation from the itching, thickening of the skin is often formed, which cracks easily. Infection of the scratch with the development of microbial complications also occurs frequently.
Causes of eczema
The emergence and development of the disease is provoked by a complex of different factors. There are primary and secondary factors.
The main reasons:
- genetic predisposition
- failure of the body’s defenses
- epidermal barrier disorders
Secondary:
- stresses;
- endocrine and gastrointestinal diseases;
- decreased immunity;
- increased sweating;
- varicose veins;
- chronic foci of infection in the body;
- use of unsuitable means for a particular person (household chemicals, perfumes, cosmetics, etc.).
Types of eczemas
True eczema
- The main symptom is the appearance of inflammatory foci with small blisters and pitting erosions, with mucous, scratching, crusting, and peeling.
- Itching and burning is pronounced.
- In addition to foci of inflammation, there are scattered dry rashes on the body.
- The boundaries of the foci are indistinct.
- Rashes appear on the face and hands, spreading to the trunk and extremities. Symmetry of the lesions is pronounced.
- The acute process turns into a chronic course, which is manifested by a cyclic development from exacerbations to relapses.
- With a prolonged course, the skin in the lesion foci thickens and the skin pattern intensifies.
Seborrheic eczema
- Subjects with oily skin and increased sebum production.
- It is localized first on the scalp.
- It is observed in places with a large number of sebaceous glands – behind the ears, in the anatomical folds, on the folds, then passes to the neck and chest.
- The affected area has small yellow and pink nodules, crusts and scales, and swollen skin.
- In the scalp area, the hair is sticky with exudate, there are scales, crusts and redness. After removal of the crusts, there are soaking spots.
- The itching is troubling.
- When skin folds are affected, cracks, swelling, and redness appear.
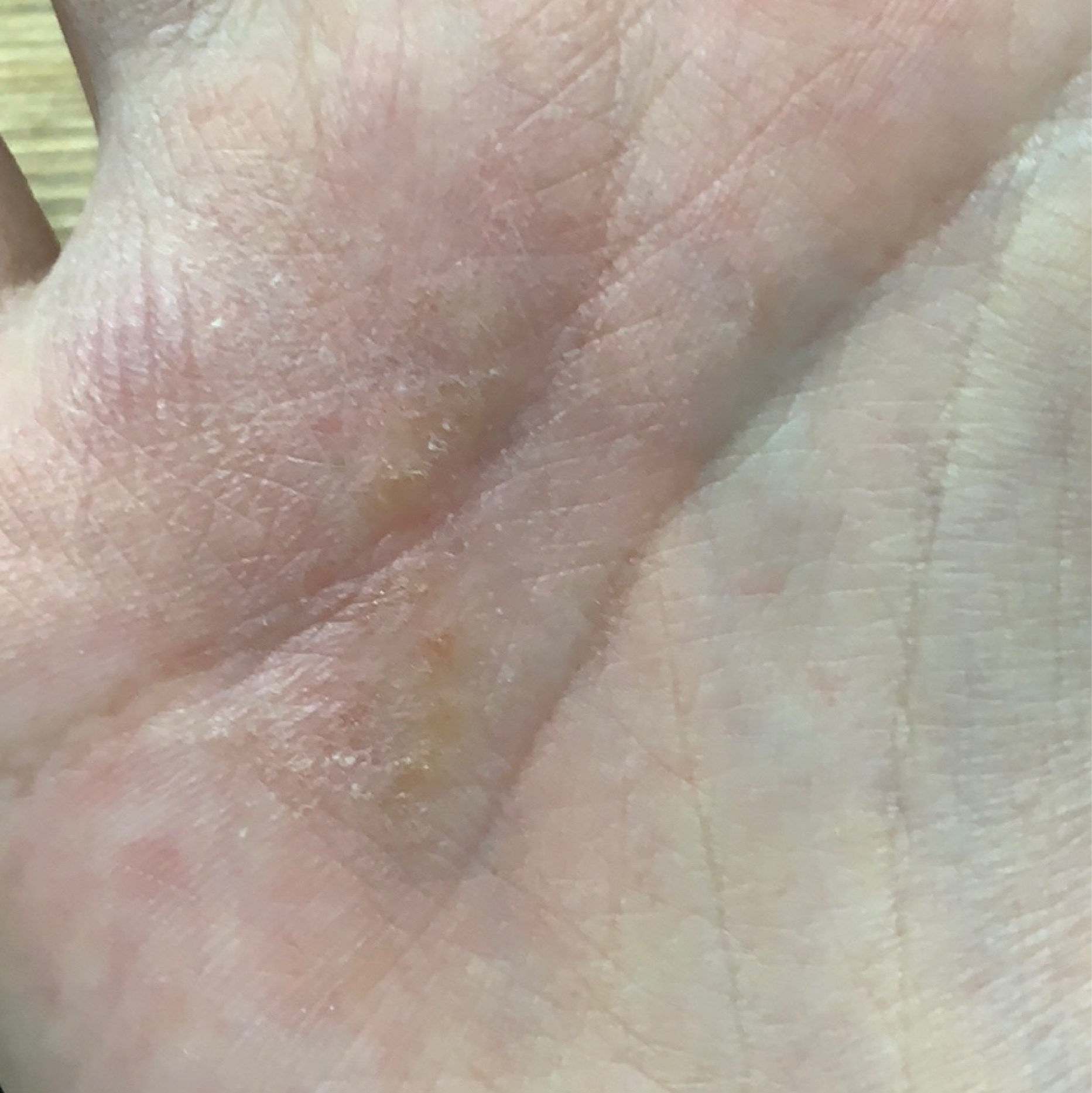
Dyshidrotic eczema
- It occurs against the background of allergic reactions.
- Exacerbations are characteristic of the spring and summer seasons or periods of great stress.
- Adults under forty years of age are more susceptible, while children are less common.
- The first symptoms affect the fingers – rashes begin to appear on the sides, and then they spread to the palms of the hands and feet.
- Burning and soreness are bothersome.
- As the disease progresses, exfoliation occurs.
Nuchal translucent eczema
- It is characterized by the formation of severely itchy red, rounded plaques that become wet during periods of exacerbation.
- It appears on various parts of the body, more often on the shins and forearms.
- Accompanied by intense itching and peeling.
- Is provoked by insect bites, scratches, dry skin, contact with nickel, disorders of blood supply to the lower extremities.
- Men are more often affected.
Microbial eczema
- It is the result of increased sensitivity of the body to a microbial agent (streptococcus, staphylococcus, etc.) when pathogens get into open wounds on the skin.
- Frequent provoking factors are disorders of the neuroendocrine and immune systems, gastrointestinal dysfunction.
- The lesions have an asymmetric shape and distinct boundaries. Purulent crusts are formed with moist areas beneath them.
- There is a strong itching sensation.
Hypostatic (varicose) eczema
- More often develops with varicose veins, obesity, heart and kidney failure, hypertension, endocrine disorders, including diabetes mellitus.
- The lower extremities are affected.
- A feeling of heaviness and pain in my legs bothers me.
- Redness and edema of the skin of the anterior surface of the shins form against a background of serous- purulent crusts with moist surfaces underneath.
Sycosiform eczema
- It occurs with a predisposition to inflammatory diseases of the hair follicles.
- It develops in places of increased hairiness – chin, upper lip, axillary area, pubis.
- The itching is troubling.
- The formation of moist areas, pustules, and crusts is observed.
Occupational eczema
- Provoked by regular contact with chemical irritants and microtraumas.
- Zones of lesions are in places of contact with irritating agents, but it is also possible throughout the body.
- The clinical picture is similar to true eczema.
- Symptoms go away after contact with irritants is stopped.
Pediatric eczema
- Causes – hereditary predisposition in combination with other factors – parasitic infections, endocrine system diseases, irrational use of drugs (antibiotics and hormones), violation of the diet and the nature of nutrition, gastrointestinal diseases, contact with chemical irritants (household products, cosmetics).
- It is very itchy.
- There is redness and swelling of the skin, the formation of small blisters, as well as extensive blotchy lesions as the disease progresses.
- With a prolonged course, the skin becomes drier and superficial cracks form.
Diagnosis
- Initial examination;
- Allergological and immunological tests;
- Laboratory tests of blood, urine, and feces;
- Skin scrapings;
- Biochemical blood tests and other additional tests as indicated.
The diagnosis is usually made clinically. Identification of atopic diseases in relatives helps to confirm the diagnosis.
Differential diagnosis is made with allergic contact dermatitis, seborrheic dermatitis, scabies, vesicles, psoriasis, pyoderma, mycosis, atopic dermatitis.
Treatment
The patient is consulted and treated by a dermatologist. Strict adherence to his recommendations can significantly improve the condition and achieve persistent remission in the chronic course of the disease.
Treatment Components:
- Drug therapy;
- Establishment and elimination of provocative factors;
- Identification and treatment of comorbidities;
- Adherence to a hypoallergenic diet and lifestyle;
- Proper skin care;
- Rational use of medical cosmetics.