Squamous cell carcinoma of the skin (SCC) is a malignant tumor of the skin with germination in the dermis and the development of severe local destruction. It has a dubious prognosis due to the fact that there is a likelihood of metastasis. Pathology usually occurs at the age of over 35-40 years, equally often in men and women.
Predisposing factors
There is no clear cause for squamous cell carcinoma. It is only appropriate to talk about predisposing factors that, to varying degrees, can increase the risk of these neoplasms:
- Excessive insolation: excessive exposure to solar ultraviolet;
- Ionizing radiation;
- The influence of chemical compounds that damage the skin;
- Chronic skin injuries;
- Some dermatological diseases: Mibelli’s porokeratosis, dystrophic bullous epidermolysis, lichen planus, lupus erythematosus, Lewandowski-Lutz epidermodysplasia;
- The role of human papillomavirus in increasing the risk of Bowen’s disease is not ruled out.
Diagnostics
The diagnosis of squamous cell carcinoma is based on a clinical examination, which includes a routine examination of the formation and dermatoscopy. After examination, a biopsy is performed.
Symptoms
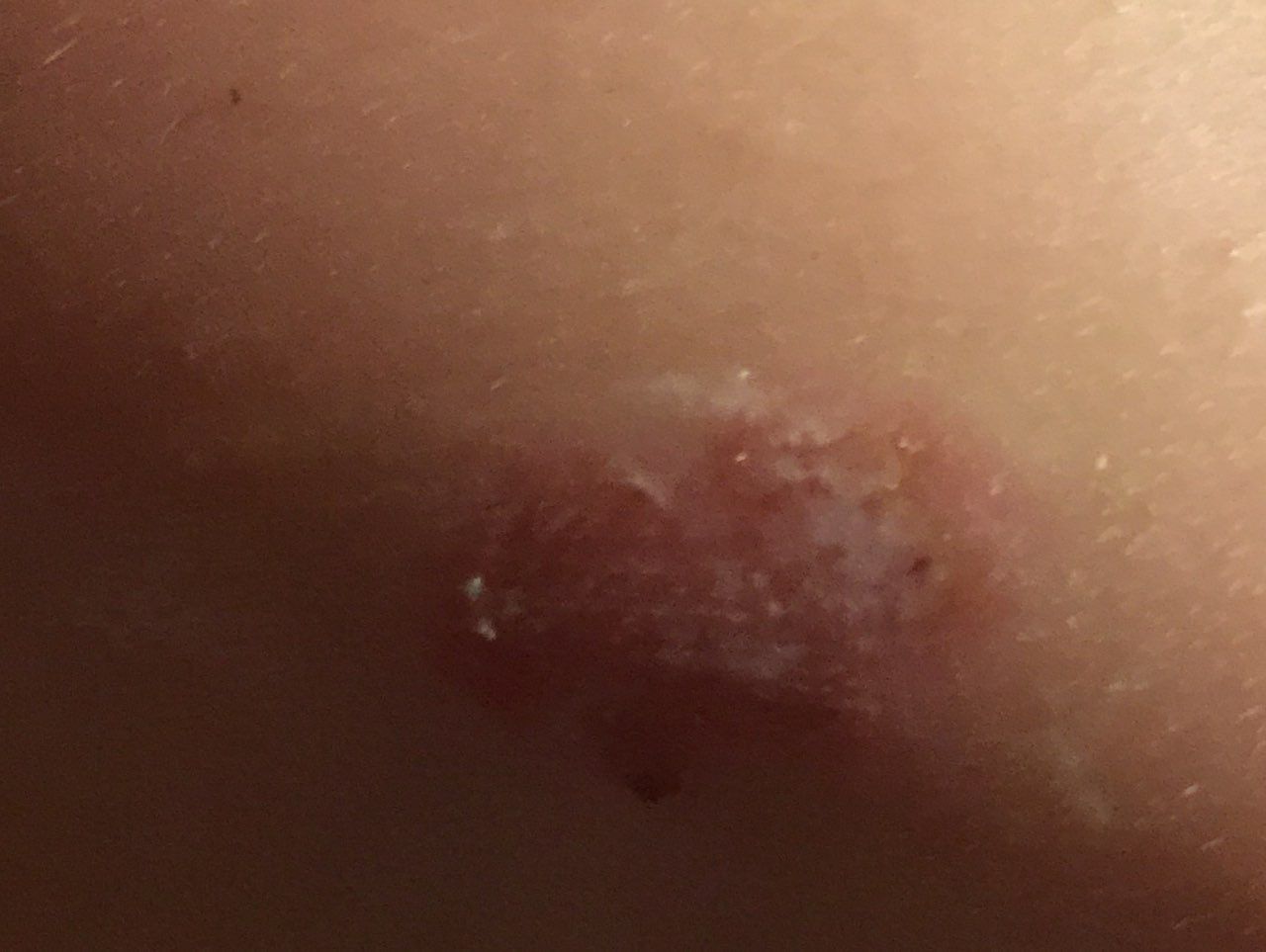
A visual examination of squamous cell carcinoma determines a plaque or flattened protrusion protruding above the skin. On the surface, there are tuberosity, wartiness, ulcerations, crusts, hyperkeratosis. Upon contact, or even with a minor injury, bleeds easily.
Borders are usually fuzzy (infiltrative growth) and uneven. The shape is often irregular, asymmetric, but sometimes the focus of squamous cell carcinoma is represented by a regular round or oval formation. It may look like a crater-like ulcer with a depression in the center (possibly even below the skin level) or vice versa, protruding above the skin and fixed to it by a wide pedicle formation.
The color is pink, pink-red, with the appearance of horny masses – gray shades join, the intensity of which depends on the severity of keratosis in the tumor area. In long-existing forms, foci of tissue necrosis with white-yellow, dirty-gray color may appear on the surface.
Hair growth is absent.
Sizes range from 4 mm to 40 mm with rapid tumor growth. In the absence of timely treatment, individual foci can reach large sizes, occupying entire anatomical areas.
On palpation, a more dense formation is defined in comparison with the surrounding skin.
Subjective sensations are usually absent. There is no morbidity with mechanical action on the tumor itself. When subcutaneous structures are involved in the tumor process, pain may appear.
Foci of squamous cell carcinoma are located mainly on the face, scalp, and neck (about 70% of all cases). The remaining proportion falls on the skin of the trunk and limbs.
Dermatoscopic Description
With dermatoscopy of squamous cell carcinoma, the following signs are visualized:
- Keratotic masses with horny overlays;
- Telangiectasia in the peripheral part of the tumor;
- Inclusions in the form of small blood clots;
- Studs and/or linear vessels;
- The radial orientation of the vascular structures in the peripheral part of the tumor;
- Glomerular structures represented by foci of convoluted vessels;
- Lack of pigmentation.
Differential diagnosis
Differential diagnosis is carried out with such neoplasms as:
- Keratoacanthoma;
- Cutaneous horn;
- Seborrheic keratosis;
- Actinic keratosis;
- Bowen’s disease;
- Basal cell carcinoma;
- Pigmentless forms of melanoma.
Risks
Squamous cell skin cancer is a malignant tumor with all the ensuing circumstances. Even after its removal, the risk of a return of the disease in the form of local relapse or the appearance of metastases remains. The later the treatment is carried out, that is, the larger the lesion focus (area, depth) by the tumor, the higher the risk of progression.
Metastases most often appear in regional (closest to the tumor) lymph nodes, but their spread to other organs cannot be ruled out.
Squamous cell carcinoma can appear both on healthy skin and on the background of existing benign or precancerous tumors. In the latter case, there is a certain degree of difficulty in timely differential diagnosis and detection of malignant transformation.
In recent years, the incidence of SCC has been increasing: by about 10% in 5 years.
Tactics
If a suspicion is detected or the first signs of squamous cell skin cancer are detected, an oncologist should be consulted. The oncologist conducts additional specifying tests. In the absence of sufficient clinical data for an unambiguous diagnosis, sometimes the tactics of active dynamic observation is chosen. More often, a suspicious lesion or biopsy is performed, followed by histological examination.
With histological confirmation of SCC, a standard list of examinations is assigned to search or exclude the presence of metastases, after which a special treatment plan is formed.
In this regard, in patients with the presence of SCC, the risk of other malignant tumors increases – a regular thorough examination of the skin is recommended. When suspicious neoplasms are detected, a positive role is played by their photo fixation, which will subsequently determine even minor changes in appearance. In the same situations, an examination by a dermatologist or oncologist in the spring and autumn (before the beach season and after it) is indicated. Of great importance is the mapping of skin neoplasms, which greatly simplifies further observation, the search for new formations, or changes to existing ones.
Treatment
The main treatment method is surgical: wide excision of the tumor focus. This is the most effective method with a low risk of local recurrence.
Another effective and universally recognized method is short-focus x-ray therapy (radiation therapy). It is usually used to treat foci up to 20 mm.
The use of other methods of local exposure (laser removal or cryodestruction) even of the earliest forms is unacceptable. The tumor should be removed radically, within healthy skin, without damaging the tumor focus itself. Otherwise, the risk of both local relapse and metastasis increases.
Today, methods are being developed for the local use of cytostatics (chemotherapy). However, there is no unequivocal opinion regarding such treatment due to the fact that these methods increase the duration of treatment of skin cancer, the cost, the damaging effect on the healthy surrounding skin and have dubious radicalism when used improperly. Such treatment should be carried out under the strict supervision of a specialist. On the other hand, local treatment with the help of certified and approved by oncologists means has a good cosmetic result.
Prevention
Prevention of the appearance of squamous cell carcinoma of the skin and its progression is gentle and careful attitude to the skin:
- Limitation of ultraviolet radiation (natural (sun) and artificial);
- The use of protective creams during periods of active sun;
- Exclusion of chronic skin trauma;
- Limitation or exclusion of ionizing radiation, occupational hazards;
- Compliance with safety measures when working with skin-damaging factors;
- Personal hygiene and basic awareness of skin tumors.
It also requires regular examination of the skin, timely consultation with a specialist in the event of external changes in skin tumors, and the removal of potentially dangerous neoplasms.