Trichomycosis is a collective term that includes a group of diseases occurring with damage to hair follicles and hair. There are the following types of trichomycosis: tineacapitis (mycosis of the scalp) and tineabarbae (mycosis of the beard area). The main cause of trichomycosis is the appearance on the skin of dermatomycete fungi of the genus Microsporum and Trichophyton.
Types of trichomycosis
Tineacapitis – dermatophytosis of the scalp and hair in this area. Refers to infectious “quarantine” mycoses, epidemic outbreaks are possible. It is caused by any pathogenic dermatophytes from the genus Trichophyton and Microsporum, with the exception of T. concentricum. M. canis is the most common pathogen in the world, followed by T. tonsurans.
Various clinical manifestations depend on the type of pathogen and the degree of the body’s immune response. There are two possible patterns of microorganism invasion:
- Ectotrix – small and large fungus spores (arthroconidia) spread outside the hair shaft;
- Endotrix – arthroconidia remain inside the hair shaft.
Clinical types of Tineacapitis
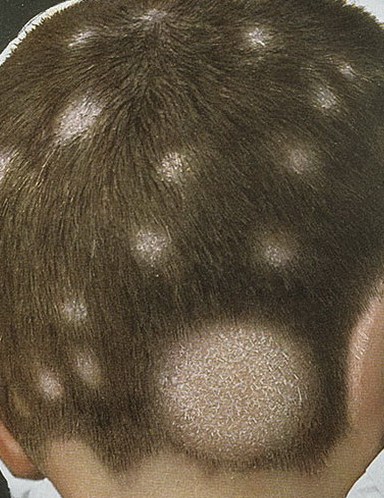
Non-inflammatory (superficial) type – usually caused by anthropophilic fungi: endotrix Tr. tonsurans (“trichophytosis”) or ectotrix M. Ferrugineum, M. Canis (“microsporia”).
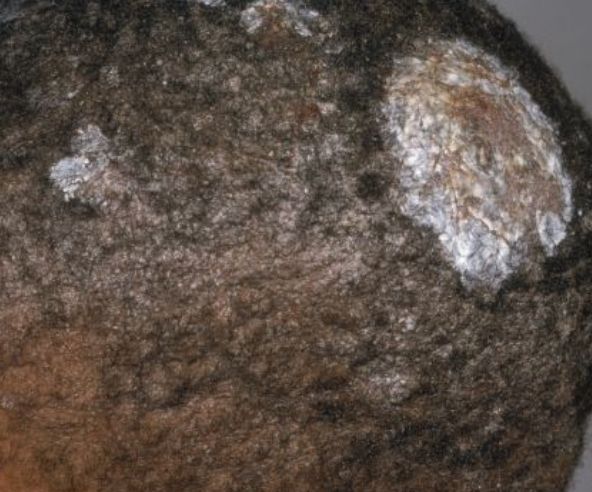
Skin: minimal inflammation (round, pink-red or dull red, well-defined patches) or absent (non-inflammatory or seborrheic type with visible flaking and hyperkeratosis). Lesions are relatively small, multiple, located in the marginal region of the scalp, but may coalesce into large areas that involve the entire scalp.
Hair can be visually intact. At the same time, the affected area often looks like a well-defined round area of alopecia (hair is broken off at the very base), hyperkeratosis and peeling are noted. The appearance resembles a “wheat field”. Preserved hair and scales emit a greenish glow in Wood’s lamp.
The inflammatory type is usually noted when infected with zoophilic Tr fungi. Gypseum and M. Canis. It manifests itself in the form of 1-3 relatively large foci of inflammation. The spectrum of inflammation ranges from pustular folliculitis to kerion, which is a deep inflammation center dotted with broken hair and follicular orifices from which pus flows. Hair can be easily removed. The consequence of this inflammation can lead to cicatricial alopecia.
Black dot dermatophytosis is caused by anthropophilic Trichophytons. This is the least inflammatory form of ringworm on the head. The affected areas are usually multiple, with uneven edges, covered with small scales. In some cases, hair loss may not occur. However, when this happens, the hair in the lesion breaks off inside the mouth, leaving black spots on the scalp. The process can lead to atrophic alopecia.
Tineabarbae – damage to the skin and hair in the area of beard or mustache growth in men. Most often caused by zoophilic microorganisms T. mentagrophytes and T. verrucosum and, in rare cases, M. canis.
Clinical types of Tineabarbae
The inflammatory type (purulent, parasitic sycosis) – usually caused by T. mentagrophytes and T. Verrucosum, completely repeats the inflammatory type of tineacapitis before the formation of kerion.
The superficial type is a form of mycosis of the beard caused by anthropophils, with a less pronounced inflammatory process, reminiscent of bacterial folliculitis with mild diffuse erythema.
Annular type – repeats tineacorporis, manifests itself as annular lesions with slightly raised inflammatory edges, covered with vesiculopustules and crusts, with central desquamation.
Diagnosis of trichomycosis
The diagnosis of trichomycosis is based on clinical evidence and epidemiological investigation. Various instrumental studies are used to confirm the diagnosis:
- Luminescent method (carried out using a special Wood lamp, emitting a special spectrum of ultraviolet illumination, in which a fungal infection of the skin and hair acquires a characteristic glow depending on the type of pathogen);
- Microscopic examination of pathological material (examination of hair or skin scales under a microscope to detect specific signs of fungal infection);
- Cultural diagnostic method;
- PCR diagnostics (study of fungal DNA in biological material).
In addition to clinical significance, accurate diagnosis and identification of the type of pathogen is necessary to determine the scope of anti-epidemic measures.
Differential diagnosis
Differential diagnosis of trichomycosis is carried out:
- Between different types of trichomycosis, depending on the pathogen;
- With alopecia areata;
- Discoid lupus erythematosus;
- Seborrheic eczema;
- Broca’s pseudopellada;
- Vulgar sycosis
- Impetiginous syphilide, etc.
Treatment of trichomycosis
When the first signs of trichomycosis appear, it is necessary to consult a dermatologist. Only in conjunction with a specialist can you choose the right treatment, which will not only avoid the progression of the disease in a given patient with the development of unpleasant complications, but also exclude the transmission of the pathogen to people around them.
For the treatment of trichomycosis, both local and systemic treatment is used. The main treatment is systemic (tablets, capsules, suspensions). Local treatment is optional. Local treatment can be independent with small lesions and the absence of pronounced clinical manifestations.
The most common antifungal drug for the treatment of trichomycosis is griseofulvin (for systemic use). The drug is quite safe, therefore it is also used in children (there is a dosage form in the form of a suspension). In addition to griseofulvin, terbinafine or itraconazole are prescribed.
With frequent episodes of trichomycosis (which indicates a weakened immune system), vitamin therapy, immunotherapy, and other drugs are prescribed to eliminate trigger factors.
With severe itching, antihistamines can be used, with the addition of a microbial infection – antibacterial drugs.
The following are used as local treatments:
- Antifungal ointments (Mikospor, Miconazole, Exoderil, Lamisil and others, including those prepared in a pharmacy);
- 2–5% iodine tincture for treatment of lesions;
- Lotions containing salicylic acid, quinosol and dimexide in the composition (prepared in the pharmacy).
In addition to medications, for the entire period of treatment, it is necessary to adhere to weekly shaving of the scalp and washing the head with hot water and soap 2-3 times a week. It is also recommended to cover your head with a gauze bandage during the day (the bandages are burned in the evening) and to minimize close contact with people, especially children, to exclude the sharing of hygiene products and clothing.